Gamified Shoulder Rehabilitation for Mild Stroke Patients Using Virtual Reality
Corresponding email: roy.navea@dlsu.edu.ph
Published at : 31 Jan 2025
Volume : IJtech
Vol 16, No 1 (2025)
DOI : https://doi.org/10.14716/ijtech.v16i1.7365
Navea, RF, Talde, VM, Armintia, FL, Cruz, SMD, Medina, G & Decena, A 2025, 'Gamified shoulder rehabilitation for mild stroke patients using virtual reality', International Journal of Technology, vol. 16, no. 1, pp. 146-159
| Roy Francis Navea | 1. Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines 2. Department of Electronics and Computer Engineerin |
| Vincent Mao Talde | Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines |
| Francisco Luis Armintia | Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines |
| Sarrah Mae Dela Cruz | Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines |
| Gabriel Medina | Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines |
| Alvin Decena | Evelyn D. Ang - Institute of Biomedical Engineering and Health Technologies, De La Salle University, 2401 Taft Ave., Manila, 0922, Philippines |
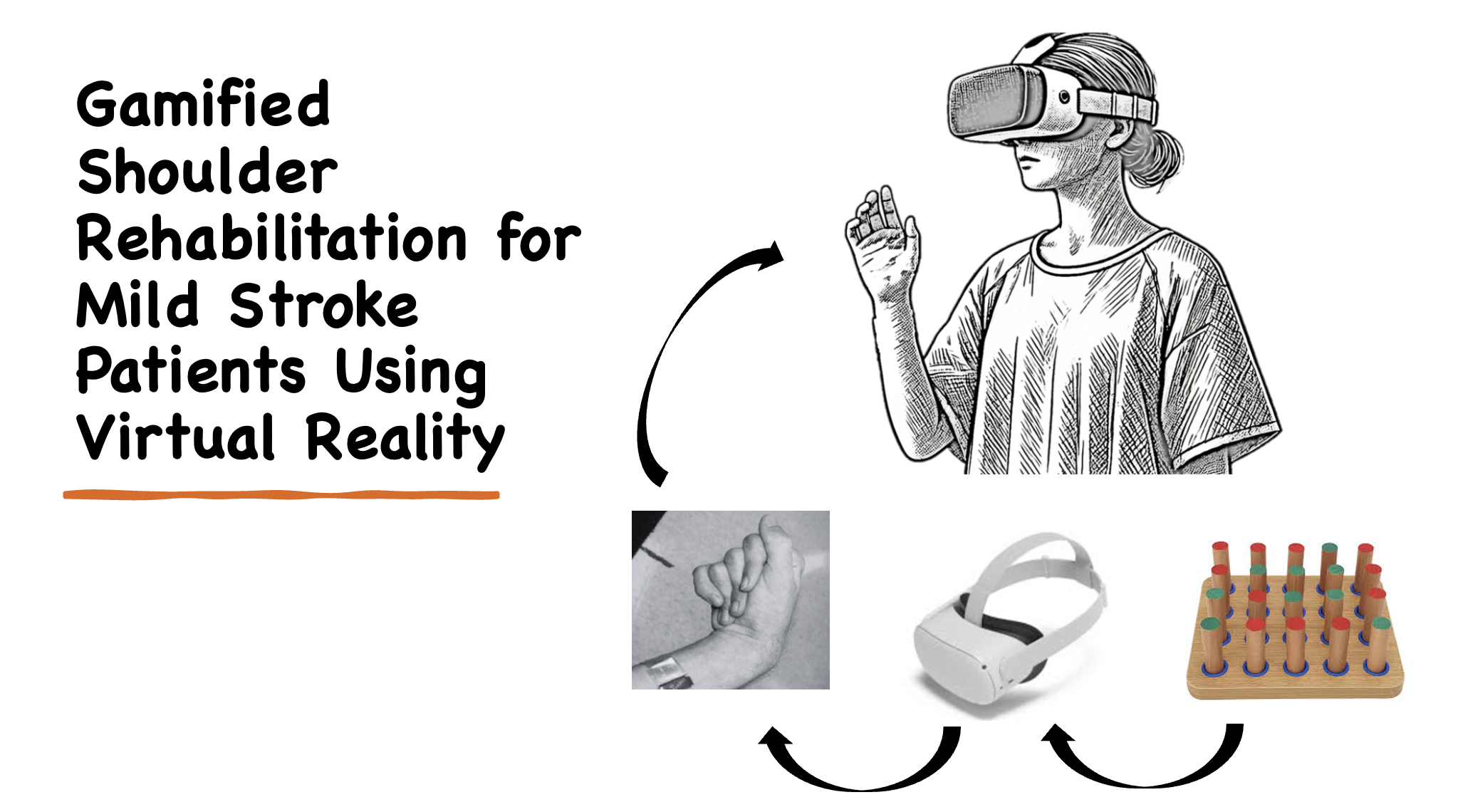
Stroke patients often encounter upper extremity impairments that necessitate rehabilitation. Traditional motor rehabilitation methods may struggle with patient adherence due to low engagement. This lack of engagement can lead to decreased motivation and, consequently, reduced participation in the rehabilitation process, which may impact the overall effectiveness of the treatment. Gamification in virtual reality (VR) adds game-like features to enhance engagement and motivation, thereby significantly improving patient involvement in rehabilitation. This study introduces i-Suksok, a VR-based game specifically designed for shoulder rehabilitation in mild-stroke patients. Created in the Unity platform, the game presents users with the challenge of maneuvering a round peg into specific holes on a pegboard using shoulder movements. It encompasses two modes: "Levels," which progressively increase in difficulty and adapt to the patient's shoulder range, and "Time Trial," where players aim to hit as many targets as possible within a designated time limit. The feedback and evaluation results from participants showed that, on average, 75% agreed with the metrics used, underscoring the significance of participant feedback and involvement in effective rehabilitation therapies, while perceptions of effectiveness, which influenced motivation and adherence, highlighted the importance of enhancing user experience in VR rehabilitation for better recovery outcomes which is supported by 69% of participant’s agreement. Gamification in VR has the potential to transform traditional methods in healthcare, education, training, and entertainment by providing an engaging, interactive experience that captures users' attention and fosters positive outcomes.
Gamification; Rehabilitation; Stroke; Upper extremity; Virtual reality
Throughout life, individuals often face illnesses, disabilities, or impairments. One of the most common causes of such conditions is stroke, which is also a leading cause of death (Salaudeen et al., 2024; Wang et al., 2023; Tsao et al., 2022). A stroke occurs when blood flow to the brain is disrupted, either by a blockage or a ruptured blood vessel. This interruption deprives the brain of oxygen and nutrients, causing tissue damage and potentially leading to tissue death if not promptly treated (Fekadu et al., 2019; Singh et al., 2013).
Stroke patients often face significant challenges during upper extremity rehabilitation due to motor impairments, which make traditional rehabilitation methods less effective. These conventional approaches frequently result in low patient motivation and adherence. However, advancements in technology, such as gamification and virtual reality (VR), have shown promise in increasing engagement and improving rehabilitation outcomes for stroke patients. Strokes are categorized by severity, with mild stroke being a common type. These typically lead to subtle motor and cognitive impairments, which can impact everyday tasks, such as returning to work. Patients may experience issues with coordination, communication, clarity of thought, impaired vision, low energy, and emotional control (Duncan et al., 2021; Scott et al., 2019). Motor impairments in the upper extremities are particularly common after a stroke. The upper extremity includes the shoulders, upper arm, forearm, and hand, consisting of 30 bones, nerves, muscles, and blood vessels (Forro et al., 2023). Hemiplegic shoulder pain is a prevalent condition affecting about 75% of stroke patients, significantly reducing their quality of life (Manurung et al., 2023; de Sire et al., 2022; Anwer and Alghadir, 2020; Dyer et al., 2020). Stroke-related shoulder impairments often lead to a decreased active range of motion (AROM), particularly in movements such as shoulder abduction, horizontal abduction, extension, forward flexion, adduction, horizontal adduction, lateral rotation, internal rotation, scapular protraction, and scapular retraction.
Traditional rehabilitation techniques for stroke recovery typically involve repetitive physical exercises under the supervision of therapists. While essential for recovery, these methods often result in low patient engagement due to their monotonous nature and the perceived lack of progress (Li et al., 2024). This disengagement can lead to reduced motivation, which is crucial for the success of rehabilitation programs (Sanchez-Gil et al., 2025). Thus, innovative strategies to sustain patient motivation and improve participation are urgently needed (Ockerman et al., 2024). Although spontaneous motor recovery may occur within the first six months after a stroke, further improvements rely heavily on consistent physical rehabilitation (Shagaeva and Shagaev, 2021; Young and Forster, 2007). Physical therapy rehabilitation is a comprehensive approach aimed at restoring, maintaining, or enhancing the physical, mental, and cognitive abilities necessary for daily activities (Buckingham et al., 2024; Mahmoud, 2021). Research indicates that physical therapy can strengthen muscles, improve quality of life, and enhance upper limb motor function (Kanika et al., 2023; Brusola et al., 2023; Teo et al., 2022; Huang et al., 2021; An and Shaughnessy 2011). Less than 35% of patients adhere to traditional rehabilitation programs, often due to limited access to services, lack of community support, and low motivation—particularly in low-to-middle-income countries (Logan et al., 2024; Asa et al., 2021). Many patients find exercises monotonous, painful, or unengaging and perceive them as ineffective. Maintaining patient engagement is critical for program adherence and success.
Gamification applies game design elements to non-game contexts, such as rehabilitation, to make exercises more engaging. By transforming routine tasks into interactive challenges, it enhances motivation and promotes better adherence (Octavia and Natasha, 2017; Deterding et al., 2011). Features like progress tracking, rewards, and feedback create a sense of accomplishment, encouraging continued participation (Tosto-Mancuso et al., 2022). Virtual reality (VR) further enhances engagement by creating immersive environments that mimic real-world scenarios. VR applications enable personalized rehabilitation experiences that adapt to a patient's needs, making exercises feel less demanding while promoting significant physical activity (Peláez-Vélez et al., 2023; Sana et al., 2023; Demeco et al., 2023; Hao et al., 2023; Truijen et al., 2022; Wu et al., 2021; Feng et al., 2019; Kalarat and Koomhin, 2019; Maggio et al., 2019; Laver et al., 2017). Integrating gamification into VR, with features like scoring and interactive challenges, offers a powerful tool for rehabilitation by sustaining patient interest and improving outcomes (Magista et al., 2018).
Several efforts have explored gamified rehabilitation (Dan, 2022; Doumas et al., 2021; Berton et al., 2020; Charles et al, 2020). Products like Neurofenix use devices like the NeuroBall to gamify hand therapy through tablet-based games. While engaging and motivational, such systems lack the immersive benefits of VR and are less effective for patients with mild impairments (Kilbride and Butcher, 2024). In contrast, VR-based rehabilitation systems, such as those using HTC Vive, show improved outcomes compared to traditional methods, though their gamification features are often limited (Mekbib et al., 2021).
Virtual reality technology offers an immersive environment that can simulate real-world scenarios for stroke patients, providing an engaging platform for rehabilitation (Laver et al., 2017). VR rehabilitation programs can be designed to adapt to individual patient needs and abilities, allowing for personalized therapy experiences (Sanchez-Gil et al., 2025). The interactive nature of VR can also reduce the perceived effort of exercises, making them feel less taxing while still promoting significant physical activity (Aderinto et al., 2023). By targeting the shoulders, the game aims to address the unique needs of this population, leveraging VR’s immersive nature and gamification principles to improve motor function and rehabilitation engagement (Büssing and Hempel, 2020). Existing research demonstrates that VR-based rehabilitation can lead to significant improvements in motor functions compared to conventional therapies, further highlighting its potential as an effective and scalable intervention (Sudiarno et al., 2024; Peláez-Vélez et al., 2023; Chen et al., 2022). This study introduces a culturally tailored VR-based game specifically designed for Filipino stroke patients with upper extremity impairments.
The i-Suksok game is designed to aid rehabilitation for individuals recovering from minor strokes, particularly those with a muscle grade of 3 to 4, and was developed through visits to rehabilitation centers where potential activities were identified and gamified, with input from rehabilitation experts to ensure alignment with real-world practices and prescribed regimens from physical therapists. The gameplay focuses on enhancing shoulder mobility through specific movements such as forward flexion, adduction, horizontal adduction (crossed flexion), and horizontal abduction, with players seated ergonomically and wearing upper limb support to isolate shoulder activity while maintaining proper posture with palms facing down. The game adapts to each player’s abilities, progressively increasing difficulty to keep them engaged and encourage continuous improvement.
The i-Suksok game incorporates core features that emphasize accessibility and replay value, including progressive difficulty, which starts with simple tasks and gradually introduces complexity as the player’s abilities improve. Customization options allow the game to adapt to individual movement ranges, accommodating varying levels of shoulder mobility, while its design motivates patients to return for regular sessions, enhancing replayability. Developed using the Unity game engine, known for its robust capabilities in creating 3D and VR applications, the game leverages the Meta Quest 2 VR headset for optimal compatibility, supporting seamless testing and iterative development. Its core functionalities are programmed in C# within Visual Studio, which integrates efficiently with Unity, enabling quick modifications and updates.
The core gameplay of the i-Suksok game revolves around the patient manipulating a cylindrical object, referred to as the “round peg,” using shoulder movements to place it into designated holes on a virtual pegboard, which is designed to mirror traditional physical therapy exercises with pegs and pegboards in a digital, VR-enabled format. The interface features a digital wooden board with multiple holes for the player to interact with, and the objective is to successfully place the cylindrical peg into specific holes, guided by a translucent indicator that highlights the target area. Once the peg is accurately placed, it locks into the hole, and the player repeats the process until all targets are completed, enhancing both engagement and therapeutic value.
The gameplay logic of the i-Suksok game, as shown in Figure 1, ensures an engaging and structured progression through its levels, beginning with a start menu where the player's score is initialized to 0, and the positions of target holes are randomized to maintain variety. As gameplay flows, the player picks up a peg and places it in the designated hole; a successful placement increases the score based on the level’s scoring system and decreases the number of remaining holes by one. This process continues with newly randomized targets until all holes are filled or the timer expires. Upon completion, if the player’s score meets or exceeds the target for the level, they progress to the next level; otherwise, they have the option to retry the level or choose to end the session, providing a balanced mix of challenge and feedback.
The development of the i-Suksok game involved regular testing with the Meta Quest 2 headset to refine gameplay mechanics, ensure alignment with rehabilitation objectives, and enhance user experience. Feedback from physical therapists and patients was integral to the design process, allowing for usability and therapeutic effectiveness improvements. The i-Suksok game represents an innovative approach to stroke rehabilitation by leveraging VR technology to gamify shoulder exercises. Its adaptive difficulty, engaging mechanics, and alignment with clinical practices create a motivating and effective tool for patients on their path to recovery.
Figure 1 Gameplay level program logic
Table 1 outlines key design considerations for the development of a game tailored for therapeutic and rehabilitation purposes, focusing on creating an engaging, effective, and accessible experience that meets the specific needs of its target audience. The game environment should closely replicate a real-world clinical setting, fostering familiarity and comfort for players through a realistic and immersive atmosphere, with a well-lit virtual room and clearly visible objects that make navigation easy. A user-friendly interface is essential, prioritizing simplicity and intuitiveness to enable effortless interaction while eliminating the need for controllers to accommodate individuals with limited motor skills or dexterity. Furthermore, the game should incorporate progress monitoring mechanisms to track the patient’s abilities before and after completing levels, providing valuable feedback to both therapists and patients regarding rehabilitation effectiveness. It must also dynamically adjust to players' capabilities, ensuring tasks are appropriately challenging with customizable difficulty levels that cater to a wide range of motor skill levels and rehabilitation needs. These design considerations aim to create a game that is enjoyable and therapeutic, ensuring that patients remain engaged while benefiting from a targeted and effective therapeutic regimen.
Table 1 Design considerations for the game.
The rehabilitation game was evaluated through a comprehensive framework aimed at determining its effectiveness in achieving therapeutic goals and assessing key parameters, including game design and overall effectiveness. The evaluation focused on several therapeutic goals, such as facilitating functional improvement in motor skills and range of motion, reducing discomfort during rehabilitation exercises, enhancing the patient’s quality of life through improved physical and emotional well-being, and fostering motivation and sustained engagement in the rehabilitation process. Game design parameters were also assessed, covering aspects like accessibility for patients with various disabilities, customization to adapt to diverse needs, a structured progression that aligns with therapy milestones, and the provision of real-time feedback to motivate patients. Effectiveness metrics included clinical outcomes, measuring the game’s impact on therapeutic improvements against baseline measurements, patient satisfaction, and comparative analysis against traditional rehabilitation methods. A total of 15 participants tested the game using a structured rating system, scoring performance across defined metrics on a scale from 1 (Strongly Disagree) to 4 (Strongly Agree). The results of this evaluation provided valuable insights into the game’s strengths and areas for improvement, guiding further development and optimization.
The development process emphasized creating a comprehensive game, starting from the initial stages of crafting VR environments and designing 3D objects as assets to incorporating a user-friendly Graphical User Interface (GUI) and refining the intricate game mechanics. Furthermore, the development also involved integrating technical analysis, specifically ensuring the accurate reading of the rotation angle, to enhance precision and reliability within the game's functionality.
3.1. Game Environment
The virtual floor, as shown in Figure 2a, was modeled after a rehabilitation center at the De La Salle Medical and Health Sciences Institute. It features a 3D rendering of a therapy room equipped with various tools, such as parallel bars, an exercise bike, a treadmill, a mat table, weights, balance balls, and steps, all designed to support diverse therapeutic needs and enhance mobility, strength, and overall physical function. These were designed to give the impression that you are in a real rehabilitation facility. Shapr3D created the 3D models in the environment, while Blender was used for game objects like the playing board and round peg, with all models built from scratch. Each object underwent UV mapping and texture baking for smooth import into Unity, maintaining optimal performance with 2K textures and no frame drops reported during gameplay, even with additional models.
Figure 2b shows the Graphical User Interface (GUI) panels that were developed using Canva and scripted in Unity to provide functionality. At the top section, there is a button that takes the user to a login screen to enter their credentials. In the bottom section, there is a "Choose a game" prompt that allows the user to select a game to play, accompanied by a grid of game tiles, each featuring a name (e.g., "I-SUKSOK Game") and other game challenges that are aimed to follow this one. Additionally, there is a "BACK" button that takes the user back to the previous screen or exits the simulation. Players are required to register when they initially launch the game.
A registration screen, as shown in Figure 2c, will appear on the screen. To facilitate patient registration, the button clicks on the keyboard are triggered by directing the reticle to an identified spot and holding it there for one to two seconds until a click event is registered.
(a) (b)
(c)
Figure 2 (a) 3D rendering of the upper extremities’ facility; (b) Game GUI; (c) Registration menu
The game is integrated with a local database, enabling the storage of important patient information regarding their score and progress. Specifically, the database records the patient’s details, such as their name and login credentials, the most recent 10 calibrations, and their scores and high scores for time-trial modes (30 seconds, 1 minute, and 2 minutes). This data is stored in a .csv file format for easy and rapid reading and writing. A method was devised to eliminate the use of Virtual Reality (VR) controllers in the VR game by incorporating a hand-tracking feature to control VR hands, benefiting patients experiencing difficulties in hand movement. The resulting game comprises two modes: Levels and Time Attack, depicted in Figure 3.
(a) (b)
Figure 3 (a) Main menu screen for the game; (b) Level selection screen
In these two modes, the player can choose whether to focus on their left shoulder or right shoulder, with progress on each shoulder being completely separate. The Levels mode comprises five distinct 'stages' that progressively increase in difficulty. Initially, only one level is accessible, and upon successful completion, a more challenging level is unlocked.
In Figure 4, there is a level selection menu displaying a 'level' that requires a specific number of holes to be hit by the end for the player to succeed. The game randomly selects which hole the patient needs to place the round peg in, and each level has a finite number of holes that must be hit. Upon selecting a hole, the game generates a silhouette of a round peg on the chosen hole to direct the player in pointing their arm toward it, while a concealed timer begins running. If the player fails to hit the hole within the given time frame, a new hole will be chosen. Failing to meet the specified number of holes in the level prevents progression to the next level.
Since each patient has distinct capabilities based on their case, the levels are custom-tailored to adapt to this by initiating an initial calibration test, depicted in Figures 4a and 4b. During this test, the patient follows a trail of the translucent round peg on the game pegboard first vertically to assess their forward shoulder flexion and then horizontally to evaluate their adduction, horizontal adduction/cross flexion, and horizontal abduction.
`
(b)
Figure 4 Calibration section (a) calibration menu, and (b) shoulder flexion calibration
This approach establishes a distinct playing area that limits the game to designate specific holes as targets, guaranteeing the patient's ability to reach them. Nevertheless, to promote progress, the game can also opt to designate a target hole beyond the patient's current capability. These challenging holes provide enough resistance to pose a greater challenge for the patient yet remain within an achievable range.
Figure 5 depicts some sample gameplays. Figure 6 shows when a level is completed and failed. These screens visually represent successful completion and instances of failure within the game.
(a) (b) (c)
Figure 5 Sample gameplay with yellow arrow pointers for user’s reference at (a) level 1, (b) level 2, and (c) level done
(a) (b)
Figure 6 Sample display for (a) level completed and (b) level failed
Figure 7 illustrates the gameplay time trial logic of i-Suksok. It involves peg placement within a specific timeframe. The steps include starting the game, placing player pegs, initializing the timer, randomizing the positions of translucent pegs, checking whether placements are within reach, displaying and starting the timer, incrementing the score upon peg placement, and repeating actions based on timer expiration until the game concludes. The game combines strategy and speed, requiring players to place pegs within designated areas within a set time limit.
Upon completing all five levels, the patient undergoes a similar test to assess improvement. Successful progress expands the playing area, returning them to level 1 with an enlarged playing area. In the event of failure, they would revert to level 1 with the same playing area. Mastery of the entire pegboard unlocks the Time Trial mode, offering the patient the choice of three time limits: 30 seconds, 1 minute, and 2 minutes. Within the chosen time limit, the patient endeavors to hit as many holes as possible. This mode, without a restricted playing area, is exclusively available to those capable of reaching any part of the board.
Figure 8a depicts the time trial selection screen, which allows the user to choose the duration of the time attack trial, with options of 30 seconds, 1 minute, or 2 minutes. While the game remains the same for the time trial, this mode features randomly placed holes all over the board without any restrictions, as shown in Figure 8b. Additionally, Figure 8c presents a sample completion of a time trial level, showcasing the score, current best score, and a single star. The rating is based on the player’s score relative to their current personal best. It awards 1 star if the score is less than half, 2 stars if it is at least half, and 3 stars if it exceeds the high score.
Visual effects in the form of particle explosions were implemented and are showcased after the round peg is inserted into the holes, serving as an indicator of task completion, as depicted in Figure 9. The background music, heard by the player during the game, was composed and created from scratch, including the sound effects triggered when the round peg is dropped and inserted into the board.
Figure 7 Gameplay time trial program logic
(b)
(c)
Figure 8 (a) Time trial selection screen; (b) Time trial play screen; (c) Time trial completed.
Figure 9 Game visuals and effects showing confetti for completed tasks
3.2. Feedback and Evaluation
Figure 10 displays the feedback and evaluation results from participants. On average, 75% agreed with the metrics, with 19% strongly agreeing and only 6% disagreeing. The disagreement may be attributed to accessibility challenges and a slight reduction in discomfort (N=15). This supports earlier work by Obembe and Eng (2016), which highlighted the importance of participant feedback in improving rehabilitation therapies. For the four metrics related to therapeutic goals, 77% agreed, 18% strongly agreed, and 5% disagreed (N=60). This is similar to the findings by Littooij et al. (2022), who noted that involving participants is key to effective rehabilitation outcomes. The research by Laver et al. (2017) emphasizes the role of participant feedback in refining VR-based rehabilitation programs. For the game design metrics, 77% agreed, 20% strongly agreed, and 3% disagreed (N=60). Lohse et al (2013) found that well-designed therapeutic games can improve user experience and rehabilitation effectiveness. This aligns with the findings by Laver et al. (2017), who demonstrated that engaging game mechanics in VR can enhance therapeutic activities. Lastly, for the effectiveness metrics, 69% agreed, 20% strongly agreed, and 11% disagreed (N=45). This echoes the work of Tatla et al. (2014), who showed that perceptions of effectiveness can greatly affect motivation and adherence. Further supporting this, Viñas-Diz and Sobrido-Prieto (2016) highlighted that enhancing the user's experience in VR rehabilitation can lead to better recovery outcomes among stroke patients.
Figure 10 Participants’ feedback and evaluation results related to effectiveness, game design, and therapeutic goals.
The i-Suksok game demonstrates the potential of virtual reality (VR) to assist stroke patients with shoulder problems by incorporating game mechanics in rehabilitation, which fosters patient engagement and addresses common challenges such as lack of motivation and difficulty that can hinder recovery. By adjusting the game's difficulty based on individual patient abilities, the developers have created a more personalized and effective tool for rehabilitation. However, despite the successful completion of the game, several limitations exist due to constrained development time. Further development is recommended, including the integration of support tools like a goniometer for accurately measuring shoulder movement angles and the inclusion of progress-tracking features to enhance clinical applicability. Since clinical trials have not yet been conducted, it is advised to consider co-designing methods with patients and stakeholders. Additionally, incorporating computer vision or AI technologies for pose and angle estimation, as well as integrating voice recognition for interacting with the game environment and introducing a virtual doctor for support and motivation, could significantly enhance the overall experience and effectiveness of the rehabilitation process.
Acknowledging the assistance of the Department of Science and Technology (DOST) of the Republic of the Philippines for its support with the research funding program of the Philippine Council for Health Research and Development (DOST - PCHRD).
Author Contributions
Roy Francis Navea contributed to the study design, supervision, conceptualization, methodology, writing, data analysis, and editing, while Vincent Mao Talde focused on gameplay, storyboarding, programming, data gathering, and writing. Francisco Luis Armintia handled programming, VR integration, and writing the discussion section, and Sarrah Mae Dela Cruz was responsible for animation, graphic design, and literature review writing. Gabriel Medina also worked on programming, gamification, and the discussion section writing, whereas Alvin Decena contributed to animation, graphic design, gameplay, and storyboarding.
Aderinto, N, Olatunji, G, Abdulbasit, MO, Edun, M, Aboderin, G & Egbunu, E 2023, 'Exploring the efficacy of virtual reality-based rehabilitation in stroke: a narrative review of current evidence', Ann Med, vol. 55, no. 2, article 2285907, https://doi.org/10.1080/07853890.2023.2285907 An, M & Shaughnessy, M 2011, 'The effects of exercise-based rehabilitation on balance and gait for stroke patients: a systematic review', The Journal of neuroscience nursing: journal of the American Association of Neuroscience Nurses, vol. 43, no. 6, pp. 298-307, https://doi.org/10.1097/JNN.0b013e318234ea24 Anwer, S & Alghadir, A 2020, 'Incidence, Prevalence, and Risk Factors of Hemiplegic Shoulder Pain: A Systematic Review', International journal of environmental research and public health, vol. 17, no. 14, article 4962, https://doi.org/10.3390/ijerph17144962 Asa, GA, Fauk, NK, Mwanri, L & Ward, PR 2021, 'Understanding Barriers to the Access to Healthcare and Rehabilitation Services: A Qualitative Study with Mothers or Female Caregivers of Children with a Disability in Indonesia', International journal of environmental research and public health, vol. 18, no. 21, article 11546, https://doi.org/10.3390/ijerph182111546 Berton, A, Longo, UG, Candela, V, Fioravanti, S, Giannone, L, Arcangeli, V, Alciati, V, Berton, C, Facchinetti, G, Marchetti, A, Schena, E, De Marinis, MG & Denaro, V 2020, 'Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients' Rehabilitation', Journal of clinical medicine, vol. 9, no. 8, article 2567, https://doi.org/10.3390/jcm9082567 Brusola, G, Garcia, E, Albosta, M, Daly, A, Kafes, K & Furtado, M 2023, 'Effectiveness of physical therapy interventions on post-stroke spasticity: An umbrella review', NeuroRehabilitation, vol. 52, no. 3, pp. 349-363, https://doi.org/10.3233/NRE-220275 Buckingham, SA, Dar Juan, AM, Demain, S, De Vera, JA, Estrada, M, Hermosura-Faeldon, L, Kent, B, Linog, MTS, Navea, RF, Jones, F 2024, 'Stroke rehabilitation in urban and rural settings in the Philippines: Protocol for an interview and visual elicitation study', PLoS ONE, vol. 19, no. 8, article e0307330, https://doi.org/10.1371/journal.pone.0307330 Büssing, A & Hempel, N 2020, 'Gamified physical rehabilitation - An example of gamification in therapy', Health Informatics Journal, vol. 26, no. 1, pp. 129-139 Charles, D, Holmes, D, Charles, T & McDonough, S 2020, 'Virtual Reality Design for Stroke Rehabilitation', Advances in experimental medicine and biology, vol. 1235, pp. 53-87, https://doi.org/10.1007/978-3-030-37639-0_4 Chen, J, Or, C & Chen, T 2022, 'Effectiveness of using virtual reality-supported exercise therapy for upper extremity motor rehabilitation in patients with stroke: Systematic review and meta-analysis of randomized controlled trials', Journal of Medical Internet Research, vol. 24, no. 6, article e24111, https://doi.org/10.2196/24111 Dan, B 2022, 'Gamification of therapy: the fun factor in rehabilitation', Developmental medicine and child neurology, vol. 64, no. 3, pp. 276-276, https://doi.org/10.1111/dmcn.15126 de Sire, A, Moggio, L, Demeco, A, Fortunato, F, Spanò, R, Aiello, V, Marotta, N & Ammendolia, A 2022, 'Efficacy of rehabilitative techniques in reducing hemiplegic shoulder pain in stroke: Systematic review and meta-analysis', Annals of physical and rehabilitation medicine, vol. 65, no. 5, article 101602, https://doi.org/10.1016/j.rehab.2021.101602 Demeco, A, Zola, L, Frizziero, A, Martini, C, Palumbo, A, Foresti, R, Buccino, G, Costantino, C 2023, 'Immersive Virtual Reality in Post-Stroke Rehabilitation: A Systematic Review', Sensors (Basel, Switzerland), vol. 23, no. 3, article 1712, https://doi.org/10.3390/s23031712 Deterding, S, Dixon, D, Khaled, R & Nacke, L 2011, 'From game design elements to gamefulness: defining gamification', 15th International Academic MindTrek Conference: Envisioning Future Media Environments, pp. 9-15, http://dx.doi.org/10.1145/2181037.2181040 Doumas, I, Everard, G, Dehem, S & Lejeune, T 2021, 'Serious games for upper limb rehabilitation after stroke: a meta-analysis', Journal of neuroengineering and rehabilitation, vol. 18, no. 1, article 100, https://doi.org/10.1186/s12984-021-00889-1 Duncan, PW, Bushnell, C, Sissine, M, Coleman, S, Lutz, BJ, Johnson, AM, Radman, M, Bettger, JPV, Zorowitz, RD & Stein, J 2021, 'Comprehensive stroke care and outcomes: time for a paradigm shift', Stroke, vol. 52, no. 1, pp. 385-393, https://doi.org/10.1161/strokeaha.120.029678 Dyer, S, Mordaunt, DA & Adey-Wakeling, Z 2020, 'Interventions for Post-Stroke Shoulder Pain: An Overview of Systematic Reviews', International journal of general medicine, vol. 13, pp. 1411-1426, https://doi.org/10.2147/IJGM.S200929 Fekadu, G, Chelkeba, L & Kebede, A 2019, 'Risk factors, clinical presentations and predictors of stroke among adult patients admitted to stroke unit of Jimma university medical center, south west Ethiopia: prospective observational study', BMC Neurology, vol. 19, no. 1, article 187, https://doi.org/10.1186/s12883-019-1409-0 Feng, H, Li, C, Liu, J, Wang, L, Ma, J, Li, G, Gan, L, Shang, X & Wu, Z 2019, 'Virtual Reality Rehabilitation Versus Conventional Physical Therapy for Improving Balance and Gait in Parkinson's Disease Patients: A Randomized Controlled Trial', Medical science monitor: international medical journal of experimental and clinical research, vol. 25, pp. 4186-4192, https://doi.org/10.12659/MSM.916455 Forro, SD, Munjal, A & Lowe, JB 2023, 'Anatomy, Shoulder and Upper Limb, Arm Structure and Function', StatPearls, StatPearls Publishing, Viewed 15 July 2024 (https://www.ncbi.nlm.nih.gov/books/NBK507841/) Hao, J, Pu, Y, Chen, Z & Siu, K 2023, 'Effects of virtual reality-based telerehabilitation for stroke patients: A systematic review and meta-analysis of randomized controlled trials', Journal of Stroke Cerebrovascular Diseases, vol. 32, no. 3, Article 106960, https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106960 Huang, J, Ji, JR, Liang, C, Zhang, YZ, Sun, HC, Yan, YH & Xing, XB 2022, 'Effects of physical therapy-based rehabilitation on recovery of upper limb motor function after stroke in adults: a systematic review and meta-analysis of randomized controlled trials', Annals of Palliative Medicine, vol. 11, no. 2, pp. 521-531, https://doi.org/10.21037/apm-21-3710 Kalarat, K & Koomhin, P 2019, 'Real-time volume rendering interaction in virtual reality', International Journal of Technology, vol. 10, no. 7, pp. 1307-1314, https://doi.org/10.14716/ijtech.v10i7.3259 Kanika, Goyal, M & Goyal, K 2023, 'Effectiveness of the physiotherapy interventions on complex regional pain syndrome in patients with stroke: A systematic review and meta-analysis', Journal of bodywork and movement therapies, vol. 35, pp. 175-181, https://doi.org/10.1016/j.jbmt.2023.04.040 Kilbride, C, Butcher, T & Warland, A 2024, 'Rehabilitation via HOMe-Based gaming exercise for the upper limb post-stroke (RHOMBUS): A qualitative analysis of participants’ experience', BMJ Open, vol. 14, no. 1, article e075821, https://doi.org/10.1136/bmjopen-2023-075821 Laver, KE, Lange, B, George, S, Deutsch, JE, Saposnik, G & Crotty, M 2017, 'Virtual reality for stroke rehabilitation', The Cochrane database of systematic reviews, vol. 11, article CD008349, https://doi.org/10.1002/14651858.CD008349.pub4 Li, Z, Lei, Y, Bui, Q, DePaul, O, Nicol, G, Mohr, D, Lee, S, Fong, M, Metts, C, Tomazin, S, Wong, A 2024, 'A digital intervention to promote self-management self-efficacy among community-dwelling individuals with stroke: Pilot randomized controlled trial', JMIR Rehabilitation and Assistive Technologies, vol. 11, https://doi.org/10.2196/50863 Littooij, E, Doodeman, S, Holla, J, Ouwerkerk, M, Post, L, Satink, T, Ter Steeg, AM, Vloothuis, J, Dekker, J & de Groot, V 2022, 'Setting meaningful goals in rehabilitation: A qualitative study on the experiences of clients and clinicians in working with a practical tool', Clinical Rehabilitation, vol. 36, no. 3, pp. 415-428, https://doi.org/10.1177/02692155211046463 Logan, A, Faeldon, L, Kent, B, Ong, A & Marsden, J 2024, 'A scoping review of stroke services within the Philippines', BMC Health Services Research, vol. 24, 1006, https://doi.org/10.1186/s12913-024-11334-z Lohse, K, Shirzad, N, Verster, A, Hodges, N & Van der Loos, HF 2013, 'Video games and rehabilitation: using design principles to enhance engagement in physical therapy', Journal of Neurologic Physical Therapy, vol. 37, no. 4, pp. 166-75, https://doi.org/10.1097/NPT.0000000000000017 Maggio, MG, Latella, D, Maresca, G, Sciarrone, F, Manuli, A, Naro, A, De Luca, R & Calabrò, RS 2019, 'Virtual reality and cognitive rehabilitation in people with stroke: an overview', The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, vol. 51, no. 2, pp. 101-105, https://doi.org/10.1097/JNN.0000000000000423 Magista, M, Dorra, BL & Pean, TY 2018, 'A review of the applicability of gamification and game-based learning to improve household-level waste management practices among schoolchildren', International Journal of Technology, vol. 9, no. 7, pp. 1439-1449, https://doi.org/10.14716/ijtech.v9i7.2644 Mahmoud Sr, IA 2021, 'Usability of telemedicine in physical therapy rehabilitation: systematic review', JMIR Rehabilitation and Assistive Technologies, https://doi.org/10.2196/25250 Manurung, JB, Lampah, C & Gessal, J 2023, 'Medical rehabilitation in post-stroke hemiplegic shoulder pain', e-CliniC, vol. 11, no. 3, pp. 306-315, https://doi.org/10.35790/ecl.v11i3.45280 Mekbib, DB, Debeli, DK, Zhang, L, Fang, S, Shao, Y, Yang, W, Han, J, Jiang, H, Zhu, J, Zhao, Z, Cheng, R, Ye, X, Zhang, J, Xu, D 2021, 'A novel fully immersive virtual reality environment for upper extremity rehabilitation in patients with stroke', Annals of the New York Academy of Sciences, vol. 1493, pp. 75-89, https://doi.org/10.1111/nyas.14554 Obembe, AO & Eng, JJ 2016, 'Rehabilitation interventions for improving social participation after stroke: a systematic review and meta-analysis', Neurorehabilitation and Neural Repair, vol. 30, no. 4, pp. 384-392, https://doi.org/10.1177/1545968315597072 Ockerman, J, Octavia, JR, Joundi, J, Penders, A, Bar-On, L, Saldien, J, 2024. ‘Matti: Tangible user interface for engaging patients in physical therapy towards a motivating rehabilitation’. International Journal of Technology. vol. 15, no. 3, pp. 697-708, https://doi.org/10.14716/ijtech.v15i3.6118 Octavia, JR & Natasha, L 2017. ‘Design of a mobile game application to support hand rehabilitation of stroke patients in Indonesia’, International Journal of Technology. vol. 8, no. 2, pp. 250-261, https://doi.org/10.14716/ijtech.v8i2.6167 Peláez-Vélez, FJ, Eckert, M, Gacto-Sánchez, M & Martínez-Carrasco, Á 2023, 'Use of virtual reality and videogames in the physiotherapy treatment of stroke patients: a pilot randomized controlled trial', International Journal of Environmental Research and Public Health, vol. 20, no. 6, pp. 4747, https://doi.org/10.3390/ijerph20064747 Salaudeen, MA, Bello, N, Danraka, RN & Ammani, ML 2024, 'Understanding the Pathophysiology of Ischemic Stroke: The Basis of Current Therapies and Opportunity for New Ones', Biomolecules, vol. 14, no. 3, article 305, https://doi.org/10.3390/biom14030305 Sana, V, Ghous, M, Kashif, M, Albalwi, A, Muneer, R & Zia, M 2023, 'Effects of vestibular rehabilitation therapy versus virtual reality on balance, dizziness, and gait in patients with subacute stroke: A randomized controlled trial', Medicine, vol. 102, no. 24, article e33203, https://doi.org/10.1097/MD.0000000000033203 Sánchez-Gil, J, Sáez-Manzano, A, López-Luque, R, Ochoa-Sepúlveda, J & Cañete-Carmona, E 2025, 'Gamified devices for stroke rehabilitation: A systematic review', Computer Methods and Programs in Biomedicine, vol. 258, https://doi.org/10.1016/j.cmpb.2024.108476. Scott, SL, Burns, SP, Schwartz, JK & Kovic, M 2019, 'Returning to work after mild stroke', Archives of Physical Medicine and Rehabilitation, vol. 100, pp. 379-383, https://doi.org/10.1016/j.apmr.2018.05.004 Shagaeva, KA & Shagaev, AS 2021, 'Neuroplasticity mechanisms and prospects for personalized rehabilitation strategies in patients with motor and cognitive impairments', Bulletin of Rehabilitation Medicine, vol. 20, pp. 37-46, http://dx.doi.org/10.38025/2078-1962-2021-20-5-37-46 Singh, B, Parsaik, AK, Prokop, LJ & Mittal, MK 2013, 'Endovascular therapy for acute ischemic stroke: a systematic review and meta-analysis', Mayo Clinic Proceedings, vol. 88, no. 10, pp. 1056-65, https://doi.org/10.1016/j.mayocp.2013.07.015 Sudiarno, A, Dewi, RS, Widyaningrum, R, Akbar, RA, Sudianto, Y, Prastyabudi, WA & Ahmadi 2024, 'Analysis of human performance and potential application of virtual reality (vr) shooting games as a shooting training simulator for military personnel', International Journal of Technology, vol. 15, no. 1, pp. 87-98 https://doi.org/10.14716/ijtech.v15i1.5303 Tatla, SK, Sauve, K, Jarus, T, Virji-Babul, N & Holsti, L 2014, 'The effects of motivating interventions on rehabilitation outcomes in children and youth with acquired brain injuries: a systematic review', Brain Injury, vol. 28, no. 8, pp. 1022-1035, https://doi.org/10.3109/02699052.2014.890747 Teo, JL, Zheng, Z & Bird, SR 2022, 'Identifying the factors affecting ‘patient engagement’ in exercise rehabilitation', BMC Sports Science, Medicine, and Rehabilitation, vol. 14, no. 18, https://doi.org/10.1186/s13102-022-00407-3 Tosto-Mancuso, J, Tabacof, L, Herrera, JE, Breyman, E, Dewil, S, Cortes, M, Correa-Esnard, L, Kellner, CP, Dangayach, N, Putrino, D 2022, 'Gamified Neurorehabilitation Strategies for Post-stroke Motor Recovery: Challenges and Advantages', Current Neurology and Neuroscience Reports, vol. 22, no. 3, pp. 183-195, https://doi.org/10.1007/s11910-022-01181-y Truijen, S, Abdullahi, A, Bijsterbosch, D, van Zoest, E, Conijn, M, Wang, Y, Struyf, N & Saeys, W 2022, 'Effect of home-based virtual reality training and telerehabilitation on balance in individuals with Parkinson disease, multiple sclerosis, and stroke: a systematic review and meta-analysis', Neurological Sciences, vol. 43, no. 5, pp. 2995-3006, https://doi.org/10.1007/s10072-021-05855-2 Tsao, CW, Aday, AW, Almarzooq, ZI, Alonso, A, Beaton, AZ, Bittencourt, MS, Boehme, AK, Buxton, AE, Carson, AP, Commodore-Mensah, Y & Elkind, MS 2022, 'Heart disease and stroke statistics—2022 update: a report from the American Heart Association', Circulation, vol. 145, no. 8, pp. e153-e639, https://doi.org/10.1161/CIR.0000000000001052 Viñas-Diz, S & Sobrido-Prieto, M 2016, 'Realidad virtual con fines terapéuticos en pacientes con ictus: revisión sistemática [Virtual reality for therapeutic purposes in stroke: A systematic review]', Neurología, vol. 31, no. 4, pp. 255-77, Spanish, https://doi.org/10.1016/j.nrl.2015.06.012 Wang, ZM, Bu, XX, Zhou, B, Li, YF & Nie, ZL 2023, 'Dietary calcium intake and the risk of stroke: Meta-analysis of cohort studies', Nutrition, Metabolism and Cardiovascular Diseases, vol. 33, no. 5, pp. 934-946, https://doi.org/10.1016/j.numecd.2023.02.020 Wu, J, Zeng, A, Chen, Z, Wei, Y, Huang, K, Chen, J & Ren, Z 2021, 'Effects of Virtual Reality Training on Upper Limb Function and Balance in Stroke Patients: Systematic Review and Meta-Meta-Analysis', Journal of Medical Internet Research, vol. 23, no. 10, article e31051, https://doi.org/10.2196/31051 Young, J & Forster, A 2007, 'Review of stroke rehabilitation', BMJ (Clinical research ed.), vol. 334, no. 7584, pp. 86-90, https://doi.org/10.1136/bmj.39059.456794.68 Zlotnik, S, Weiss, PLT, Raban, DR & Houldin-Sade, A 2023, 'Use of Gamification for Adult Physical Rehabilitation in Occupational Therapy; A Novel Concept?', Hong Kong Journal of Occupational Therapy, vol. 36, no. 2, pp. 51-56, https://doi.org/10.1177/15691861231179037
